Overtesting and overtreatment
Introduction
In June 2020, Hôpital de La Tour became the first private health care facility in the Swiss region of Romandy to partner with Smarter Medicine – Choosing Wisely Switzerland.
Hôpital de La Tour is therefore committed to the principle that a treatment should only be given if it provides a clear benefit to the patient.
As a result, several medical procedures that are potentially harmful for patients when prescribed unnecessarily were identified: prescribing certain drug classes (antibiotics, proton-pump inhibitors, and benzodiazepines), blood tests, blood transfusions, urinary catheters, and medical imaging examinations that use radiation. For each of these procedures, indicators have been developed to monitor the prescription rate or the duration.
Why are these indicators important?
The indicators below concern medical procedures. The objective is not to eliminate them but only to use them when there is a real added value for the patient.
Key indicators
1. Benzodiazepine prescriptions
Benzodiazepines are too often prescribed in hospital to treat insomnia. In Switzerland, it is estimated that one in every five patients will be given benzodiazepines during their hospital stay. However, large-scale studies show that the risk of falls and fractures can more than double in elderly people who are taking benzodiazepines and other sedative-hypnotic drugs.
This potential harm should be considered when deciding the treatment plan for insomnia, agitation, or delirium. Benzodiazepines should only be used for alcohol withdrawal symptoms, delirium tremens, and severe generalized anxiety disorders that have not responded to other treatments.
2. PPI prescriptions
Proton-pump inhibitors (PPIs) are among the most prescribed medications in Switzerland. However, it is estimated that between 30% and 50% of PPI prescriptions are not needed. PPIs are overprescribed due to off-label use outside of the established indications, the failure to reassess treatment during transitions between care settings, and rebound effects that are poorly tolerated by patients during withdrawal. The indication for using PPIs should be reviewed during each transition in care, for example by following good clinical practice guidelines to avoid unnecessarily exposing patients to known side effects, such as Clostridium difficile infections during hospitalization and upon returning home.
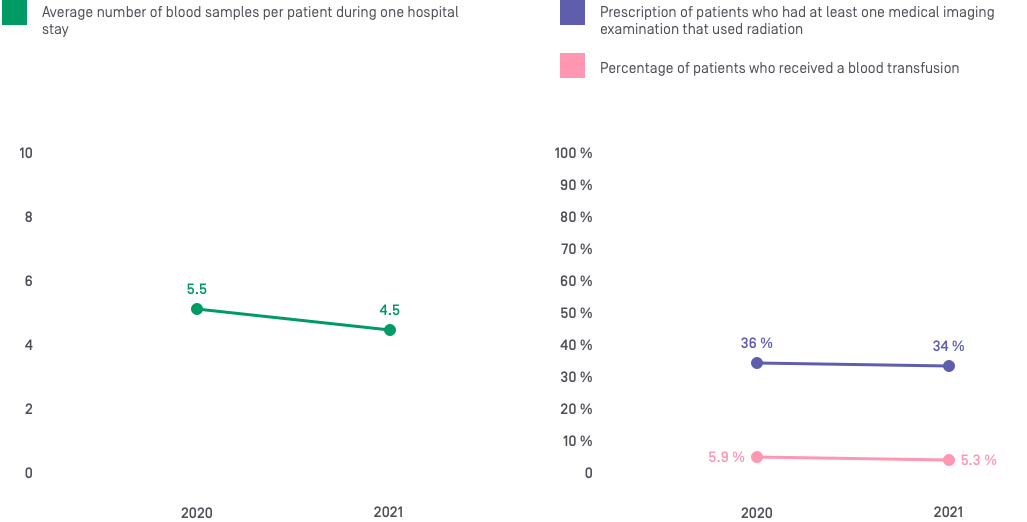
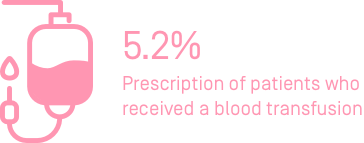
3. Blood transfusions
In line with international guidelines, a liberal transfusion strategy is not only unnecessary but may be harmful in certain situations. Blood transfusions are associated with a risk of infection and allergic reaction as well as hemodynamic risks. The use of this limited and expensive resource should therefore be optimized. International guidelines recommend a restrictive transfusion strategy, with a transfusion threshold of 70–80 g/L, except in special cases. The clinician should always use single-unit red blood cell transfusions and clinically reassess and check hemoglobin levels before administering a second transfusion. This does not apply to hemorrhaging patients.
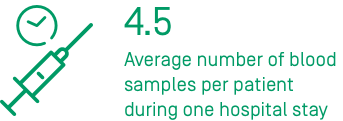
4. Repeated blood tests
Multiple laboratory tests are prescribed regularly, sometimes even on a daily basis. Yet, laboratory tests should only be requested if the result can be used to meet a specific clinical need. Regularly prescribing tests increases health care costs and is not beneficial to patients, with the potential to even harm them due to the detrimental side effects, such as pain when drawing blood, anemia, and a series of unnecessary further tests caused by a false-positive result.
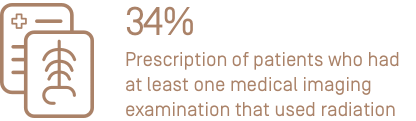
5. Medical imaging examinations
Medical imaging examinations expose patients to potentially toxic doses of radiation. These examinations are only necessary if they are used to meet a clinical need and when an alternative examination that uses no radiation is not available. For example, a study in Geneva found that over half of abdominal X-rays performed in emergency departments are prescribed unnecessarily. This examination has a radiation dose that is nearly equivalent to that of a low-dose CT scan and often does not provide enough information to help the clinician make an appropriate care plan.
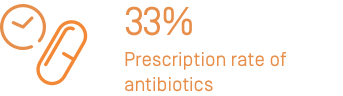
6. Antibiotics
Several studies have shown that nearly half of antibiotic treatments prescribed in a health care setting are not indicated, have a spectrum of activity that is too broad, or are prescribed for too long. Using a treatment for too long unnecessarily exposes patients to an increased risk of complications, such as Clostridium difficile infections, while misusing and overusing antibiotics accelerate antibiotic resistance in the general population and form poor preventive practices. Guidelines must be strictly followed to reduce these negative consequences.
Medications
Medical material
Measures taken towards improvement and educational interventions
In addition to an internal awareness campaign, the doctors prescribing these procedures take part in continuing medical education (CME) programs and have access to dashboards to help them compare their prescription rates with those of their colleagues. This combination of increased awareness and education therefore encourages doctors to question their practice and consider the benefit to the patient before each prescription.