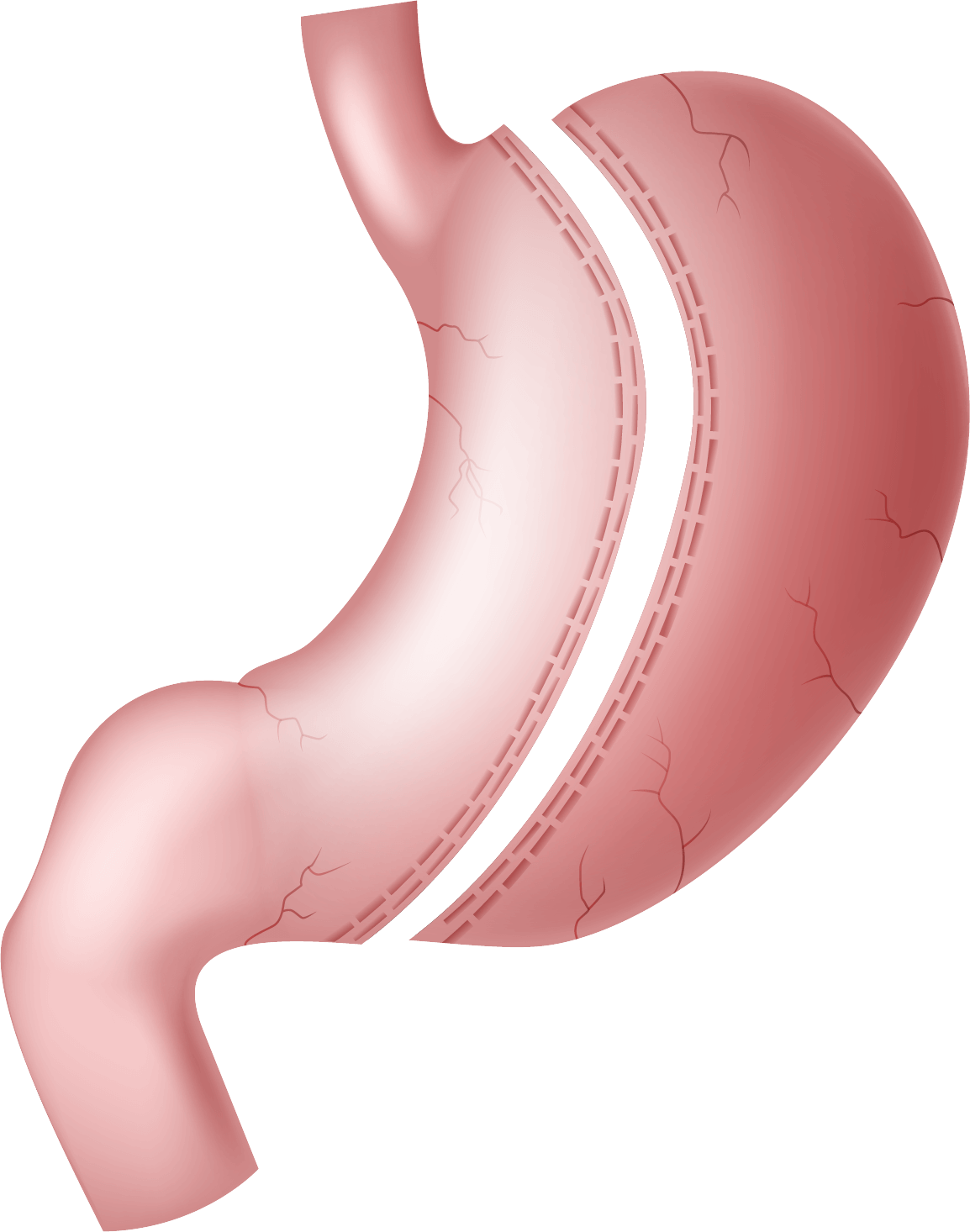
Is sleeve gastrectomy reversible?
No, this procedure is irreversible. It involves permanently removing a large part of the stomach, making it impossible to return to the original anatomy. However, other procedures may be considered at a later date in the event of complications or failure, such as conversion to gastric bypass
Will I feel hungry after the operation?
Most patients experience a marked decrease in appetite after surgery. This is due to the reduction in the production of ghrelin, a hormone responsible for the feeling of hunger, which is produced in the part of the stomach that is removed
Is there a risk of nutritional deficiencies?
Yes, but they are less common than with other procedures, such as bypass surgery. However, the reduction in the amount of food ingested requires vitamin and mineral supplementation, particularly vitamin B12, iron, calcium, and vitamin D. Regular biological monitoring is essential
Will I have to change my diet?
Yes, your post-operative diet will evolve gradually, in several phases. You will start with clear liquids, then blended foods, before returning to solid foods. This dietary journey will be supported by a team of healthcare professionals specializing in nutrition.