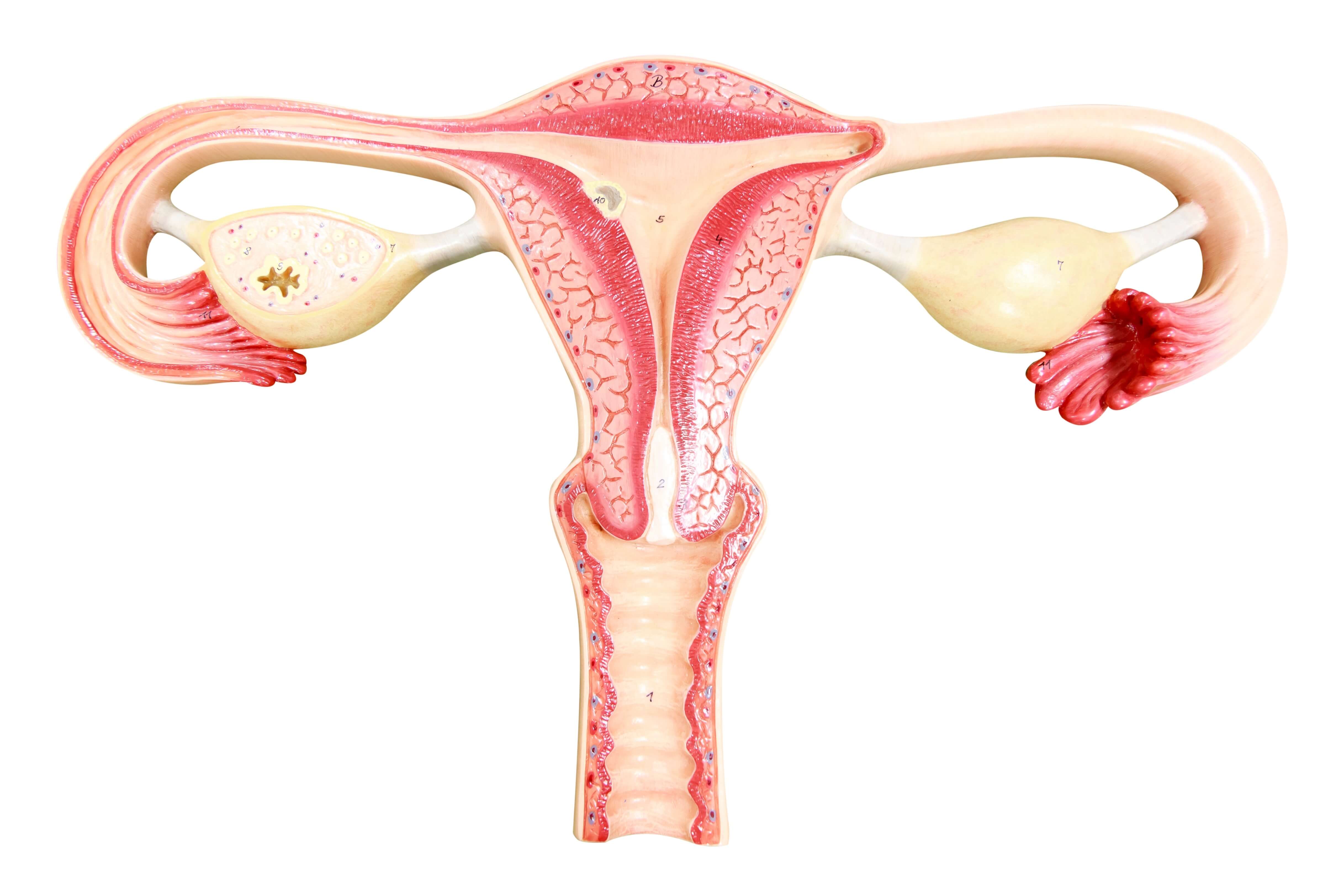
Uterus anatomy
The uterus is a hollow organ located in the female pelvis. It consists of three main parts:
Corpus uteri: The largest part of the uterus, where the fetus develops during pregnancy.
Fundus: The part of the uterus furthest from the cervix. During childbirth, the fundus helps the uterus contract.
Cervix: The lower part that connects the uterus to the vagina.
The uterine lining is made up of three layers:
Myometrium : The outer muscular layer, needed to expel the baby during childbirth or to evacuate menstrual periods during menstruation.
Endometrium: The inner mucous membrane that changes during the menstrual cycle. Endometrial cancer starts in this inner lining of the uterus.
Perimeter or serous membrane: A thin layer enveloping the body of the uterus.
Symptoms of endometrial cancer
Endometrial cancer often manifests itself with early symptoms, which means it can usually be diagnosed at an early stage. The main warning sign is abnormal vaginal bleeding. Given that endometrial cancer most often affects women after the menopause, it is bleeding in these women that should alert them most. In women of childbearing age, vaginal bleeding outside the menstrual period can also be a symptom of endometrial cancer, but this is rarer. In these women, abnormal bleeding is frequent, and most often occurs at the beginning and end of the reproductive period, corresponding to ovulatory dysfunction.
Other, less specific symptoms may also occur:
- Pelvic pain
- A feeling of heaviness in the lower abdomen
- Difficulty in urinating or frequent urination.
These symptoms are not specific to endometrial cancer and can be caused by other benign conditions. However, their appearance, particularly post-menopausal bleeding, should always prompt prompt medical attention for a thorough examination.
Causes of endometrial cancer
The exact cause of endometrial cancer is unknown, but it occurs when cells in the uterine lining undergo genetic changes that disrupt their normal life cycle.
These genetic alterations can affect various genes involved in regulating cell growth and division. These genetic alterations can be influenced by a variety of factors, including hormonal and environmental factors. Prolonged exposure to estrogen without the compensatory effect of progesterone plays a crucial role in the development of many endometrial cancers.
Risk factors of endometrial cancer
The main risk factors include:
Obesity: Obese women have higher estrogen levels due to the conversion of androgens by adipose tissue. The higher the body mass index (BMI), the greater the risk.
Age: as with most cancers, age is an important risk factor. The majority of cases occur in women between the ages of 75 and 79.
Diabetes: in cases of type 2 diabetes, insulin resistance and consequent hyperinsulinism promote endometrial cell carcinogenesis. Women with type 1 diabetes are also at increased risk, but the causal mechanism is less clearly identified.
Duration of hormone exposure: early puberty and late menopause are risk factors because of the longer exposure to estrogen
Hormone replacement therapy: the use of estrogen without progesterone (menopausal hormone therapy) increases the risk of endometrial cancer.
Certain hormone therapies: used in particular to treat breast cancer (tamoxifen).
Family history: such as endometrial cancer, colon cancer and ovarian cancer.
Polycystic ovary syndrome (PCOS): causes hormonal imbalances that increase risk.
Lynch syndrome: is associated with a high risk of endometrial cancer, in addition to colorectal and ovarian cancer.
Diagnosis of endometrial cancer
Diagnosis of endometrial cancer is based on a combination of clinical and imaging examinations, followed by histological confirmation.
Ultrasound: to examine the uterus and measure the thickness of the endometrium, to detect any abnormalities.
Hysteroscopy (endoscopy of the uterus): to visualize the uterine cavity using a small camera inserted through the cervix.
Endometrial biopsy: removal of a sample of endometrial tissue for microscopic analysis, which can be performed during hysteroscopy.
Magnetic resonance imaging (MRI) and computed tomography (CT): used to determine the extent of the disease and plan treatment.
Classification
Two main types of endometrial cancer are now recognized, each with distinct molecular characteristics and prognosis:
Type 1 (endometrioid) tumors, which occur most frequently and are the least aggressive. This type is easy to treat.
Type 2 (non-endometrioid) tumors are less frequent but more aggressive.
The stage of the cancer then describes its size and degree of spread.
This classification is important because it influences the choice of treatment and the prognosis of the disease.
Endometrial cancer treatments
The management of endometrial cancer is mainly based on surgery, often combined with other complementary treatments. The choice of treatment depends on a number of factors, including the stage of the disease, histological type, tumour grade, the patient's age and general condition.
Surgery
Total hysterectomy (removal of the uterus), with or without bilateral adnexectomy (removal of the fallopian tubes and ovaries), is the first-line treatment.
Advantages: Eliminates the primary tumour and reduces the risk of recurrence.
Disadvantages: Invasive procedure with a significant recovery period and permanent effects such as surgical menopause in the case of adnexectomy.
Radiotherapy
Uses radiation to destroy remaining cancer cells after surgery or to treat inoperable tumors.
Advantages: Reduces the risk of local recurrence.
Disadvantages: Side effects such as fatigue, redness or skin irritation and gastrointestinal disorders.
Chemotherapy
Uses drugs to kill cancer cells, often as a complement to surgery and radiotherapy.
Benefits: Useful for advanced or metastatic cancers. Reduces the risk of recurrence.
Disadvantages: Severe side effects include dry mucous membranes, nausea, vomiting and alopecia.
Hormonal therapy
Uses hormones or drugs to block the effect of natural hormones on cancer cells.
Advantages: Less invasive than surgery and can be used to treat early-stage cancers. Temporary solution in less advanced cases, for women wishing to preserve their fertility.
Disadvantages: May not be effective for all types of cancer, and may cause hormonal side-effects.
Immunotherapy
Uses the patient's immune system to recognize and attack cancer cells.
Advantages: may be effective for certain cancers refractory to conventional treatments.
Disadvantages: may cause autoimmune side effects.
Evolutions and possible complications
The prognosis for endometrial cancer is generally good when detected at an early stage. However, certain complications may arise:
- Local or distant recurrence.
- Metastases (spread to other organs).
- Treatment-related complications.
Regular follow-up is essential for early detection of any recurrence.
Preventing endometrial cancer
Although not all cases can be avoided, certain measures can reduce the risk:
Maintaining a good weight: reduces the risk associated with obesity.
Regular physical activity: contributes to a healthy weight, hormonal balance and reduced cardiovascular and metabolic risks.
Cautious use of hormone therapy: medical consultation to balance the benefits and risks of hormone therapy after menopause. Always combine progesterone with estrogen therapy.
Regular medical supervision: especially for women with a family history or other high-risk factors.
When should you contact the doctor?
Vaginal bleeding after menopause, unusual menstrual bleeding (between cycles or excessively heavy periods), persistent pelvic pain and unexplained weight loss warrant medical consultation.
Care at Hôpital de La Tour
Multidisciplinary and highly specialized care
Given the complexity of the disease, care for patients with endometrial cancer involves several stages and several medical specialties. Hôpital de La Tour boasts an experienced multidisciplinary team on a single site. Our gynecologists, radiologists, surgeons, radiotherapists, oncologists and specialized nurses work together to define the best therapeutic strategy to provide the best care for patients. Thanks to our state-of-the-art technical facilities, treatments are targeted and minimally invasive, enabling patients' quality of life to be preserved as much as possible.
Personalized care
At Hôpital de La Tour, we recognize that cancer affects everyone differently, both physically and emotionally. A dedicated nurse ensures that each woman receives personalized care. As a result, each patient's care pathway is built as closely as possible around the concerns and needs of the patient and her family. We offer patients a wide range of resources and supportive care to help them make the most of their treatment and maintain an optimal quality of life.
FAQ sur le cancer de l'endomètre
What are the main symptoms of endometrial cancer?
The main symptom of endometrial cancer is vaginal bleeding in post-menopausal women, or bleeding outside the menstrual period in women of childbearing age.
What is the prognosis for endometrial cancer?
The prognosis for endometrial cancer is favorable if the diagnosis is made at an early stage, with a 5-year survival rate of 80%.
How is endometrial cancer treated?
Total hysterectomy is the gold standard. Radiotherapy or chemotherapy may be offered after this surgical treatment. For certain early-stage cancers, hormone therapy may be offered to women wishing to preserve their fertility. Immunotherapy may be offered in certain cases for the most advanced cancers, or if other solutions are unsuitable.
Can contraception protect against endometrial cancer?
Hormonal contraception can help reduce the risk of endometrial cancer.
Can endometrial cancer be prevented?
You can reduce your risk of developing endometrial cancer by knowing the symptoms and your own risk factors, and by taking action against modifiable risk factors. Regular physical activity and maintaining a healthy weight are recommended to reduce the risk of cancer as well as cardiovascular disease.